When the dream of holding a little one slips away too soon, the silence behind can be louder than words. Miscarriage is not just a medical term; it is a heartbreak that touches millions of women and families around the world. The loss of a pregnancy before the 20th week, known as a miscarriage, is a far more common experience than often discussed, affecting an estimated 1 in 4 recognised pregnancies. This medical event is not a single entity but occurs in several forms, each with distinct characteristics. These forms include threatened miscarriage, incomplete and missed miscarriage.

Types of Miscarriage
A threatened miscarriage involves symptoms like vaginal bleeding, with the cervix remaining closed, and the pregnancy may still continue. An inevitable or incomplete miscarriage involves significant bleeding and cramping, where the cervix has now opened and some, but not all, pregnancy tissue has passed. Finally, a missed miscarriage is a particularly poignant type where the embryo has stopped developing. The body may still not have recognised the loss, which is often discovered during a routine ultrasound without symptoms.
What Causes a Miscarriage?
Among the miscarriages that occur in the first trimester, about half result from a chromosomal abnormality. These genetic abnormalities prevent the embryo from developing properly. In these cases, the miscarriage doesn’t happen because you did anything “wrong”—it was simply the result of an abnormality.
In the second trimester, chromosomal and structural abnormalities of the fetus can contribute to miscarriage. But at this stage, a miscarriage is more commonly associated with other problems, such as malformation of the uterus, the development of growths in the uterus (called fibroids), uterine infection, and certain medical conditions.
Other factors that can cause or contribute to miscarriage include:
- Significant radiation exposure
- Bacterial infections that can inflame the lining of the uterus
- Certain chronic medical conditions, like unmanaged diabetes and thyroid problems
- Excessive drug or alcohol use
- Hormone problems
- Immune system disorders, including lupus
- Older parental age (chromosomal abnormalities are more likely to occur in the eggs and sperm of people over 35)
- Smoking
While not all miscarriages can be prevented, proactive steps can significantly optimise health for a future pregnancy. The foundation of this is preconception care, which involves consulting a gynaecologist before trying to conceive. This allows for managing chronic conditions, reviewing medications, and starting essential supplements (most critically high-dose folic acid) as early as possible to support fetal development from the very first moments. Once pregnant, diligent antenatal care is crucial. Attending all scheduled visits allows for early detection and management of potential issues, providing the best possible chance for a healthy, full-term pregnancy.
Management of miscarriages
Following a diagnosis, a gynaecologist will discuss management options tailored to the specific type of miscarriage and the patient’s health. There are 3 primary approaches to management. These include expectant management, medical, and surgical management.
Management Options for Miscarriage: Expectant, Medical, and Surgical
Expectant management involves allowing the body to pass the tissue naturally over time. This method can be successful but can take some time to complete and involves experiences like heavy bleeding and strong cramps. Medical management, on the other hand, utilizes medications such as misoprostol to induce contractions and expel the tissue. Mifepristone helps block the hormone needed to maintain pregnancy. Surgical management, also known as Manual Vacuum Aspiration (MVA) or Dilation and Curettage (D&C), is a minimally invasive procedure to gently remove any remaining tissue from the uterus. The choice depends on factors such as gestational age, the amount of bleeding, and the patient’s emotional and physical preferences, with the core goal being a complete and safe resolution to prevent infection.
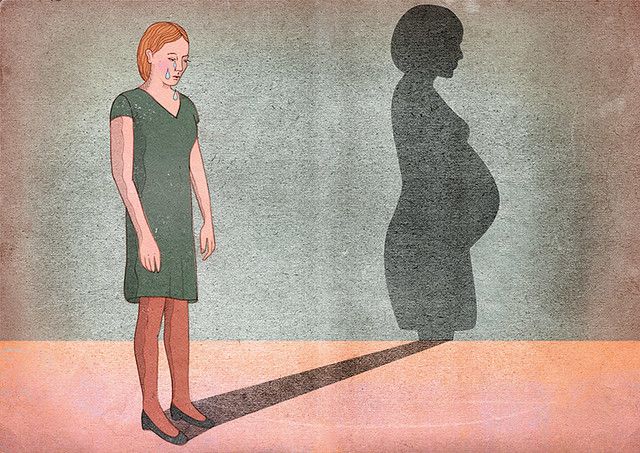
Emotional Impact of Miscarriage
The emotional toll of a miscarriage is profound and unique to each individual and family. For the woman, it is a devastating physical and psychological event, often accompanied by feelings of profound grief, guilt, and a sense of failure. The loss is not just of a pregnancy, but of the dreams, hopes, and future envisioned for that child. Partners also grieve deeply, and the experience can place significant strain on a relationship as each person may process the grief differently. This collective sorrow is frequently compounded by a culture of silence, leaving many to suffer in isolation, unsure how to articulate their pain or seek support.

Miscarriage Prevention
In the painful aftermath of a loss, consulting a gynaecologist is also a critical step toward understanding the cause and helping to prevent recurrence. A healthcare provider can ensure that the miscarriage is managed completely and safely. Furthermore, they can order tests to investigate potential underlying causes, such as uterine abnormalities, autoimmune disorders, untreated infection, trauma, or genetic factors. While many miscarriages are caused by chromosomal abnormalities that are random and unlikely to repeat, identifying a treatable issue can provide a clear pathway to a healthier future pregnancy. This proactive medical partnership offers not just clinical care but immense hope and emotional reassurance to grieving parents, transforming a sense of helplessness into empowered action for the future.
Ultimately, miscarriage is not a reflection of a woman’s worth or ability to carry a child. It is a deeply human experience that deserves compassion, understanding, and acknowledgment. By shedding light on it, we honor the silent grief many carry and remind them they are not alone.